
Back ما قبل الإرجاج Arabic تسمم الحمل ARZ প্ৰি-এক্লাম্পছিয়া Assamese Hamiləlik toksikozu Azerbaijani پری-ایکلامپسیا AZB Прееклампсия Bulgarian প্রি-এক্লাম্পসিয়া Bengali/Bangla Preeklampsija BS Preeclàmpsia Catalan Cyn-eclampsia Welsh
| Pre-eclampsia | |
|---|---|
| Other names | Preeclampsia toxaemia (PET) |
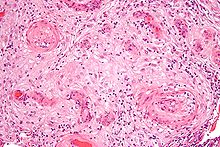 | |
| A micrograph showing hypertrophic decidual vasculopathy, a finding seen in gestational hypertension and pre-eclampsia. H&E stain. | |
| Specialty | Obstetrics |
| Symptoms | High blood pressure, protein in the urine[1] |
| Complications | Red blood cell breakdown, low blood platelet count, impaired liver function, kidney problems, swelling, shortness of breath due to fluid in the lungs, eclampsia[2][3] |
| Usual onset | After 20 weeks of pregnancy[2] |
| Risk factors | Obesity, prior hypertension, older age, diabetes mellitus[2][4] |
| Diagnostic method | BP > 140 mmHg systolic or 90 mmHg diastolic at two separate times[3] |
| Prevention | Aspirin, calcium supplementation, treatment of prior hypertension[4][5] |
| Treatment | Delivery, medications[4] |
| Medication | Labetalol, methyldopa, magnesium sulfate[4][6] |
| Frequency | 2–8% of pregnancies[4] |
| Deaths | 46,900 hypertensive disorders in pregnancy (2015)[7] |
Pre-eclampsia is a multi-system disorder specific to pregnancy, characterized by the new onset of high blood pressure and often a significant amount of protein in the urine or by the new onset of high blood pressure along with significant end-organ damage, with or without the proteinuria.[8][1][9][10] When it arises, the condition begins after 20 weeks of pregnancy.[2][3] In severe cases of the disease there may be red blood cell breakdown, a low blood platelet count, impaired liver function, kidney dysfunction, swelling, shortness of breath due to fluid in the lungs, or visual disturbances.[2][3] Pre-eclampsia increases the risk of undesirable as well as lethal outcomes for both the mother and the fetus including preterm labor.[11][12][3] If left untreated, it may result in seizures at which point it is known as eclampsia.[2]
Risk factors for pre-eclampsia include obesity, prior hypertension, older age, and diabetes mellitus.[2][4] It is also more frequent in a woman's first pregnancy and if she is carrying twins.[2] The underlying mechanisms are complex and involve abnormal formation of blood vessels in the placenta amongst other factors.[2] Most cases are diagnosed before delivery, and may be categorized depending on the gestational week at delivery.[11] Commonly, pre-eclampsia continues into the period after delivery, then known as postpartum pre-eclampsia.[13][14] Rarely, pre-eclampsia may begin in the period after delivery.[3] While historically both high blood pressure and protein in the urine were required to make the diagnosis, some definitions also include those with hypertension and any associated organ dysfunction.[3][10] Blood pressure is defined as high when it is greater than 140 mmHg systolic or 90 mmHg diastolic at two separate times, more than four hours apart in a woman after twenty weeks of pregnancy.[3] Pre-eclampsia is routinely screened during prenatal care.[15][16]
Recommendations for prevention include: aspirin in those at high risk, calcium supplementation in areas with low intake, and treatment of prior hypertension with medications.[4][5] In those with pre-eclampsia, delivery of the baby and placenta is an effective treatment[4] but full recovery can take days or weeks.[13] The point at which delivery becomes recommended depends on how severe the pre-eclampsia and how far along in pregnancy a woman is.[4] Blood pressure medication, such as labetalol and methyldopa, may be used to improve the mother's condition before delivery.[6] Magnesium sulfate may be used to prevent eclampsia in those with severe disease.[4] Bed rest and salt intake have not been found to be useful for either treatment or prevention.[3][4]
Pre-eclampsia affects 2–8% of pregnancies worldwide.[4][17][12] Hypertensive disorders of pregnancy (which include pre-eclampsia) are one of the most common causes of death due to pregnancy.[6] They resulted in 46,900 deaths in 2015.[7] Pre-eclampsia usually occurs after 32 weeks; however, if it occurs earlier it is associated with worse outcomes.[6] Women who have had pre-eclampsia are at increased risk of high blood pressure, heart disease and stroke later in life.[15][18] Further, those with pre-eclampsia may have a lower risk of breast cancer.[19]
- ^ a b Eiland E, Nzerue C, Faulkner M (2012). "Preeclampsia 2012". Journal of Pregnancy. 2012: 586578. doi:10.1155/2012/586578. PMC 3403177. PMID 22848831.
- ^ a b c d e f g h i Al-Jameil N, Aziz Khan F, Fareed Khan M, Tabassum H (February 2014). "A brief overview of preeclampsia". Journal of Clinical Medicine Research. 6 (1): 1–7. doi:10.4021/jocmr1682w. PMC 3881982. PMID 24400024.
- ^ a b c d e f g h i "Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists' Task Force on Hypertension in Pregnancy" (PDF). Obstetrics and Gynecology. 122 (5): 1122–1131. November 2013. doi:10.1097/01.AOG.0000437382.03963.88. PMC 1126958. PMID 24150027. Archived (PDF) from the original on 2016-01-06. Retrieved 2015-02-17.
- ^ a b c d e f g h i j k l WHO recommendations for prevention and treatment of pre-eclampsia and eclampsia. World Health Organization. 2011. hdl:10665/44703. ISBN 978-92-4-154833-5. Archived (PDF) from the original on 2015-05-13.
- ^ a b Henderson JT, Whitlock EP, O'Connor E, Senger CA, Thompson JH, Rowland MG (May 2014). "Low-dose aspirin for prevention of morbidity and mortality from preeclampsia: a systematic evidence review for the U.S. Preventive Services Task Force". Annals of Internal Medicine. 160 (10): 695–703. doi:10.7326/M13-2844. PMID 24711050. S2CID 33835367.
- ^ a b c d Arulkumaran N, Lightstone L (December 2013). "Severe pre-eclampsia and hypertensive crises". Best Practice & Research. Clinical Obstetrics & Gynaecology. 27 (6): 877–884. doi:10.1016/j.bpobgyn.2013.07.003. PMID 23962474.
- ^ a b Wang H, et al. (GBD 2015 Mortality and Causes of Death Collaborators) (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/s0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- ^ Phipps EA (1 May 2019). "Pre-eclampsia: pathogenesis, novel diagnostics and therapies". Nature Reviews Nephrology. 15 (5): 275–289. doi:10.1038/s41581-019-0119-6. PMC 6472952. PMID 30792480.
- ^ Hypertension in pregnancy. ACOG. 2013. p. 2. ISBN 978-1-934984-28-4. Archived from the original on 2016-11-18. Retrieved 2016-11-17.
- ^ a b Lambert G, Brichant JF, Hartstein G, Bonhomme V, Dewandre PY (2014). "Preeclampsia: an update". Acta Anaesthesiologica Belgica. 65 (4): 137–149. PMID 25622379.
- ^ a b Magee LA, Nicolaides KH, von Dadelszen P (May 2022). Longo DL (ed.). "Preeclampsia". The New England Journal of Medicine. 386 (19): 1817–1832. doi:10.1056/NEJMra2109523. PMID 35544388. S2CID 248695137.
- ^ a b Laule CF, Odean EJ, Wing CR, Root KM, Towner KJ, Hamm CM, et al. (October 2019). "Role of B1 and B2 lymphocytes in placental ischemia-induced hypertension". American Journal of Physiology. Heart and Circulatory Physiology. 317 (4): H732 – H742. doi:10.1152/ajpheart.00132.2019. PMC 6843018. PMID 31397167.
- ^ a b Martin N (2018-08-14). "Trusted Health Sites Spread Myths About a Deadly Pregnancy Complication". ProPublica. Lost Mothers. Archived from the original on 2021-05-15. Retrieved 2021-05-28.
From the Mayo Clinic to Harvard, sources don't always get the facts right about preeclampsia. Reached by ProPublica, some are making needed corrections.
- ^ Martin N, Montagne R (2017-05-12). "The Last Person You'd Expect to Die in Childbirth". ProPublica. Lost Mothers. Archived from the original on 2019-06-21. Retrieved 2021-05-28.
The death of Lauren Bloomstein, a neonatal nurse, in the hospital where she worked illustrates a profound disparity: The health care system focuses on babies but often ignores their mothers.
- ^ a b Steegers EA, von Dadelszen P, Duvekot JJ, Pijnenborg R (August 2010). "Pre-eclampsia". Lancet. 376 (9741): 631–644. doi:10.1016/S0140-6736(10)60279-6. PMID 20598363. S2CID 208792631.
- ^ Bibbins-Domingo K, Grossman DC, Curry SJ, Barry MJ, Davidson KW, Doubeni CA, et al. (April 2017). "Screening for Preeclampsia: US Preventive Services Task Force Recommendation Statement". JAMA. 317 (16): 1661–1667. doi:10.1001/jama.2017.3439. PMID 28444286. S2CID 205091250.
- ^ Ananth CV, Keyes KM, Wapner RJ (November 2013). "Pre-eclampsia rates in the United States, 1980–2010: age-period-cohort analysis". BMJ. 347 (nov07 15): f6564. doi:10.1136/bmj.f6564. PMC 3898425. PMID 24201165.
- ^ Brown MC, Best KE, Pearce MS, Waugh J, Robson SC, Bell R (January 2013). "Cardiovascular disease risk in women with pre-eclampsia: systematic review and meta-analysis". European Journal of Epidemiology. 28 (1): 1–19. doi:10.1007/s10654-013-9762-6. PMID 23397514. S2CID 13239431.
- ^ Innes KE, Byers TE (November 1999). "Preeclampsia and breast cancer risk". Epidemiology. 10 (6): 722–732. doi:10.1097/00001648-199911000-00013. JSTOR 3703514. PMID 10535787.